Download the Prostate Cancer Centre's printable PDF booklets to read offline.
Prostate Cancer - General information
Prostate Cancer - Brachytherapy
Prostate Cancer - Radical Prostatectomy
Prostate Cancer - External Beam Radiotherapy
Use the Prostate Cancer Centre's treatment selector to get an idea of what treatment is right for you.
Select this link to view the treatment selector
©The Prostate Cancer Centre UK Ltd 2005. All rights reserved.

Brachytherapy
Brachytherapy is a technique for treating prostate cancer, using tiny radioactive seeds of Iodine-125 (I125) that are inserted permanently into the prostate gland. ‘Brachy’ means close and, in this treatment, the radioactivity is inserted directly into the cancerous organ. This is unlike conventional external beam radiotherapy, where it travels through the body tissues before reaching the prostate gland. Brachytherapy provides a higher, more localised radiation close to the prostate and minimises the effects on the surrounding tissues, such as the rectum and bladder.

The seeds are tiny canisters of Titanium (4.5mm long by 0.8mm diameter) which contain the radioactive isotope Iodine-125. The half-life of radioactive Iodine-125 is approximately 60 days, which means that most of the radiation is released from the seeds into the prostate gland over the first 3 months. They continue to be biologically active for about 9 months in total. After that, they become effectively inactive.
The latest techniques for brachytherapy were developed in the mid-1980s with the arrival of sophisticated ultrasound probes. These devices enable the accurate implantation of seeds into the prostate, allowing high doses of radiation to be delivered to the cancerous gland.
There are now long-term results from patients who were treated up to 15 years ago, which show that this form of treatment is highly effective in treating and curing patients with early prostate cancer.
Brachytherapy appears to be as effective as other conventional treatments, such as surgery (radical prostatectomy) or external beam radiotherapy, but with a lower side-effect profile. However, brachytherapy is not the only effective treatment for prostate cancer and some patients may be better suited by other methods of treating their prostate cancer.
Select this link to compare treatments with the Prostate Cancer Centre Treatment selector
Patients ideally suited for brachytherapy are those for whom there is a good chance that their cancer is confined to the prostate and has not spread outside of the gland. Occasionally, where it is thought there is a higher likelihood that the prostate cancer may have spread to the tissues surrounding the gland, patients will be offered a shortened five-week course of external beam radiotherapy prior to undergoing a brachytherapy implant. This combination therapy allows a greater margin of tissue around the prostate to be treated.
The brachytherapy team will advise you whether your prostate cancer is suitable for treatment by brachytherapy. Suitable patients will normally have the following characteristics:
- The PSA (Prostate-Specific Antigen) level should ideally be less than 20ng/ml at the time of their diagnosis.
- The stage of the cancer should be either T1 or T2 on rectal examination, indicating a prostate cancer confined to the gland.
- The grade of the cancer should ideally be a Gleason score of 7 out of 10 or less.
- Patients should not suffer with severe urinary symptoms, such as a very weak stream or difficulty emptying their bladder.
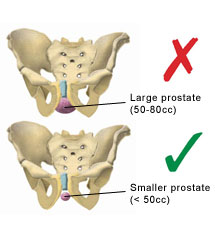
Ideally, the prostate should be relatively small – less than 50cc. If the gland is too large, areas of the prostate may be shielded by the bony skeleton, preventing an adequate implant being performed.
Patients who have had previous prostate surgery, such as a TURP (transurethral resection of the prostate), are usually best treated by an alternative therapy (e.g. radical prostatectomy or conformal external beam radiotherapy).
Once referred to the brachytherapy team for assessment as to your suitability for this treatment option for your prostate cancer, you will be sent an outpatient appointment, along with a booklet and an information video.
At your outpatient visit, you may see many members of the brachytherapy team, including both the Consultant Urologist and Consultant Oncologist at the same visit, or you may need to attend for a further outpatient appointment to ensure that you see both Consultants.
- A general history will be taken as to previous illnesses, operations, medication, etc.
- You will have a rectal examination carried out to assess the stage of the cancer. You will also undergo a painless transrectal ultrasound (TRUS) to assess the size of the prostate.
- You will be asked to complete a short questionnaire to assess your urinary symptoms, and to come to the clinic with a comfortably full bladder. This is because a flow rate and bladder scan to measure the residual volume of urine left behind after voiding will be performed.
- Discussion of the stage and grade of your cancer will take place, as well as your suitability for prostate brachytherapy.
Following your visit, if you are suitable for brachytherapy and are happy to proceed with this as a treatment option for your prostate cancer, the Brachytherapy Co-ordinator will then be able to schedule your potential dates.
An application for funding from your primary care trust may be necessary, if the procedure is to be carried out on the NHS. This can take several weeks and, unfortunately, not all applications are successful. If not, then you will have the option to appeal to your primary care trust or to self-fund your treatment. We can assure you that we will help to fight your cause as strongly as possible.
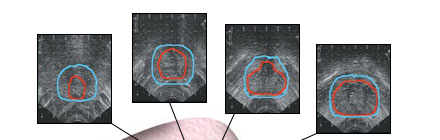

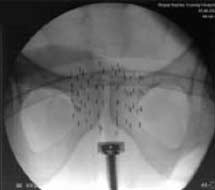
Key: Red line = prostate; Blue line = limit of radiation to be delivered
Prostate brachytherapy is carried out as a two-stage technique, with Stage 1 being The Volume Study and Stage 2 being The Implantation Process of the seeds, which is carried out approximately 4 weeks later.
Stage 1 – the volume study
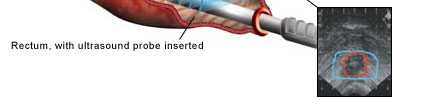
This is a detailed transrectal ultrasound, normally performed as a day-case procedure under general anaesthetic. You should not drive for 24 hours afterwards and will need to be accompanied home by a responsible adult.
You will need to have bowel preparation the day before the procedure, to ensure that the rectum is empty, so that clear ultrasound images of the prostate can be obtained. You will be sent a sachet of Picolax powder to mix with water and to drink the day before. It is important that you drink plenty of water both the day before and for 48 hours afterwards to re-hydrate yourself.
During the volume study, a catheter is placed in the water pipe (urethra) whilst under anaesthetic. This will help to identify this structure during the procedure. The catheter will be removed before you wake from the anaesthetic. You may find that you pass some jelly from the penis after the scan and you may notice some slight discomfort during the first time that you pass urine.
The prostate volume is outlined on the ultrasound images, including the position of the urethra.

A three-dimensional model is then constructed by the brachytherapy planning computer and a dose plan produced. This plan will be unique to each patient and will determine the position and number of seeds needed. The seeds are then ordered for each individual patient.
Occasionally, if the prostate gland is too large (between 50-80cc), you may need to have a course of hormone therapy for 3 months, in order to shrink the prostate down to a size that will then be suitable for the seed implant.
Research is currently in progress to allow the volume study to be performed in the out-patient clinic, avoiding the need for a general anaesthetic.
Stage 2 – the implantation process
You will be admitted on the day of the procedure. As for the Volume Study, a sachet of Picolax will be sent to you, to be taken the day before the implant, in order to clear the bowel.
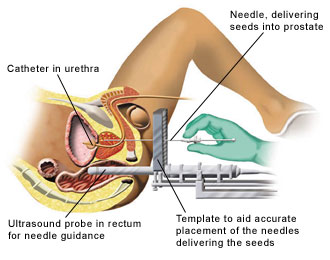
The procedure is performed under a general anaesthetic in the operating theatre. Radioactive Iodine seeds are inserted under transrectal ultrasound guidance, using needles that pass through the skin between the legs behind the scrotum (the perineum). Each needle may deliver between 2-6 seeds and, normally, 20-30 needles are required to deliver between 80-120 seeds. Most of the seeds implanted are woven into a strand of absorbable material to help maintain their position and they will remain in place permanently.
A catheter is again placed into the urethra whilst you are under anaesthetic. This remains in place for a few hours after the procedure, until the effects of the anaesthetic have fully worn off. X-rays are taken throughout the procedure, to check the position of the seeds.
CT scan
You will have a CT scan either directly following your implant, or early the following morning. This procedure will allow us to check the position of the seeds, to ensure that an adequate radiation dose has been delivered. It is an essential part of the ongoing audit process of our brachytherapy programme. However, in over 500 cases, we have never had cause to re-implant further seeds. Your catheter will be removed once you have had your CT scan.
Immediate
Immediately after the operation, you may notice some bruising beneath the scrotum and tenderness between the legs. You will have an ice bag placed between your legs whilst in the recovery room, to help reduce this bruising and discomfort.
Once the catheter has been removed, you may notice some discomfort when passing urine. While in hospital, your urine will be filtered, to ensure that any loose seeds that you may pass are caught. This event is rare and usually will happen within the first 24 hours following implant.
We will ensure that you are able to pass urine satisfactorily before you are discharged home.
A small percentage of patients (approximately 5%) may hold a significant residual amount of urine in their bladder immediately after the implant. This may result in either requiring a catheter to be left in place for a week, or being taught how to pass a fine catheter themselves for a period of time. This is normally only for two weeks or less, until normal voiding returns.
It is quite common to see some blood in the urine for a day or two after the procedure. This is quite normal, so do not be alarmed.
Advice on drinking

For one week after the implant, you are encouraged to drink plenty of water to flush through any small blood clots that may develop out of the bladder. Thereafter, you should return to a normal drinking pattern and your daily intake should not normally exceed 1.5 litres per day.
It is important that you avoid all caffeinated drinks (tea, coffee, coke) in the first few months after the implant, as these are likely to aggravate your urinary symptoms. However, alcohol, in moderation, is fine.
You may also find that cranberry juice is helpful. 1-2 glasses per day is enough.
Urinary symptoms

After the implant, it is common for patients to notice a gradual worsening of their urinary symptoms. Often, patients will find that they do not have too many problems during the first couple of weeks following implant. Symptoms will then peak at around 4-6 weeks post-implant, but improve over the ensuing months. For this reason, we would normally advise that you do not travel outside of the UK for the first
2-4 weeks following the implant
Typically, patients complain of a slow stream, with urinary frequency and urgency during the day and night. There may also be a feeling of incomplete emptying of the bladder, with the need to strain. Most often, the symptoms are worse at night and during periods of inactivity.
These side-effects are due to the swelling of the prostate following the procedure and irritation of the prostate and bladder lining due to radiation from the seeds. They are temporary and will settle in time.
We would normally expect that by 6-9 months following implant a patient’s urinary symptoms will have returned to how they were before treatment began.
Medications
After the brachytherapy implant, all patients will receive:
- An alpha-blocker, such as tamsulosin (Flomax®) or alfuzosin (Xatral®).
- An anti-inflammatory painkiller, such as diclofenac sodium (Voltarol®).
- A course of antibiotics, usually ciprofloxacin, for one week.
Alpha-blocker
This tablet relaxes the muscle within the prostate gland and helps to reduce the narrowing of the water pipe as it runs through the swollen prostate, so reducing urinary symptoms. This is best taken in the early evening.
You will be encouraged to take this tablet for at least
3-6 months after the implant and you should get a repeat prescription from your GP.
Anti-inflammatory painkiller
This tablet has two benefits. It is an effective painkiller and is also useful in reducing the inflammation from the swollen prostate gland, so helping to relieve urinary symptoms. You will receive a one-week supply of this tablet from the hospital. Some patients find that they may require a longer course of this medication and this can usually be obtained from your GP.
Antibiotic
You will receive a one-week course of antibiotics, such as ciprofloxacin. These will help to prevent infection following the implant. They are safe to take with an alcoholic drink if desired.
Urinary retention
As previously mentioned, approximately 1 in 20 patients may have temporary difficulty in emptying their bladder after the implant and this can result in urinary retention.
The symptoms of urinary retention are an inability to pass urine and lower abdominal discomfort, usually with a constant desire to urinate. Should this occur, we suggest that you either contact us or, in a painful emergency situation, it may be necessary to contact your GP or local A & E department.
In the first instance, you will merely need to have a catheter inserted into your bladder to drain the retained urine. Normally, however, we do prefer to teach patients to catheterise themselves, using single-use disposable catheters, which most patients find is easier and more convenient. This avoids having a permanent, indwelling catheter. The inability to pass urine is usually transient and, within a few weeks, you will find that your bladder starts to empty properly again and the need for catheterisation will stop.
Bowels
Some patients find that, immediately following the implant, their bowels tend towards constipation. This can usually be relieved by an increase in fresh fruit, vegetables and fibre.
Occasionally, patients can experience troublesome rectal symptoms following their implant, such as frequency of opening their bowels or diarrhoea. This symptom is more common following additional external beam radiotherapy than with a brachytherapy implant alone.
The symptoms are usually self-limiting and can often be managed by changing one’s diet slightly, by reducing the roughage, i.e. decreasing fruit and fibre intake. Immodium medication can further reduce any urgency or discomfort. Very occasionally, steroid suppositories are required. These symptoms tend to start 6 months after the implant.
Erectile dysfunction

Erection of the penis may be affected by brachytherapy. The risk is lower in younger men who have had no previous difficulties obtaining an erection and it tends to affect about 25% of our patients following treatment.
Current research suggests that the risk is lower than with other treatments, such as radical prostatectomy. Treatment with tablets, such as Viagra, is usually effective in approximately 80% of patients, should difficulties in achieving and sustaining an erection occur. Some men notice a decreased or dry ejaculate following brachytherapy. This is a common, temporary, side-effect of Flomax, but can also occur as a result of the brachytherapy implant itself.
Follow-up after Brachytherapy
Patients will be regularly reviewed in clinic and their PSA will be first checked 3 months after the implant. Usually, it will then be checked every 3 months for the first year and every 6 months thereafter. Approximately 25% of patients will experience a temporary small rise in PSA (a ‘PSA bounce’), typically anywhere between 6 months-2 years after the procedure. This is quite common, with the PSA dropping again after a few months. The reasons for this bounce phenomenon are unclear, but it does not have any effect on the overall success of the treatment.
Resuming normal physical activities
You should be able to resume normal activities (e.g. work, shopping) within a few days. However, we would normally advise you to avoid heavy lifting or strenuous activity for the first two weeks after your implant.
Many patients are concerned about whether an implant poses any potential dangers of radiation exposure to their family and friends. It is important to remember that although the seeds are radioactive, you are not. Objects that you touch or items that you use do not become radioactive. Other people may use linen, clothing, tableware, or dishes after you without special precautions. Your bodily waste (urine and stool) are not radioactive.

There are no restrictions on travel or physical contact with other adults. However, special precautions listed below should be taken when in contact with small children and pregnant women in the first 2 months following treatment.
Family relations
You may sleep in the same bed as your partner, provided she is not pregnant. Sexual intercourse, using a condom, may be resumed after 1 month, once you feel comfortable to do so. Initially, a condom should be used, because there is a very small risk that a seed may be passed in the semen.
Your semen may be discoloured dark brown or black. This is normal and is a result of bleeding that may have occurred during the implant. Following 2-3 ejaculations, it will not be necessary to use a condom.
Radiation protection
There are no formal restrictions on your activities when you return home. However, we recommend that the following precautions are followed for the first 2 months after the implant, after which time the radiation levels reduce significantly and you may resume life as normal.
- Women who are or may be pregnant should not sit very close to you (e.g. on the same sofa or bed) for more than a few minutes a day. However, you may continue to greet or hug them as you would have done before the implant and spend as long as you wish in the same room as them.
- Do not sit children on your lap for long periods. As explained above, you may briefly cuddle them for a few minutes and they may stay in the same room as you for as long as you wish.
- Other adult family, friends and colleagues are not at risk and restrictions on time and activities are not necessary.
What happens if the cancer returns?
Whilst the success rate of brachytherapy seems to be as high as for surgery, neither treatment option can guarantee cure. Should the cancer return in the prostate gland, a radical prostatectomy, cryotherapy or high-intensity focused ultrasound (HIFU) are possible further treatment options that can still provide cure.
The Prostate Cancer Centre has prepared a short video containing useful information on Prostate Brachytherapy. The video is designed to help you understand the Brachytherapy procedure in more detail and to hear the views of other men who have already undergone the treatment.
Select this link to view the Prostate Cancer Centre videos
If you would rathere not watch the video online then you can obtain a copy (in DVD or VHS Video format) directly from the Prostate Cancer Centre by selecting this link and completing the form.
Brachytherapy is a very effective treatment for early prostate cancer, with patients rapidly returning to normal activities.
Urinary incontinence after this procedure is rare (less than 1%) and the risk of impotence seems lower than with surgery and external beam radiotherapy.
Patients do, however, experience a temporary deterioration in their urinary symptoms for the first 6 months or so after their implant.
It is important to remember that the day you are discharged from hospital after the implant is really the day that your radiotherapy treatment starts.
We have collected stories from our patients who have undergonesome of the treatments offered at the Prostate Cancer Centre.






