Download the Prostate Cancer Centre's printable PDF booklets to read offline.
Prostate Cancer - General information
Prostate Cancer - Brachytherapy
Prostate Cancer - Radical Prostatectomy
Prostate Cancer - External Beam Radiotherapy
Use the Prostate Cancer Centre's treatment selector to get an idea of what treatment is right for you.
Select this link to view the treatment selector
©The Prostate Cancer Centre UK Ltd 2005. All rights reserved.

![]()
Prostate Cryotherapy
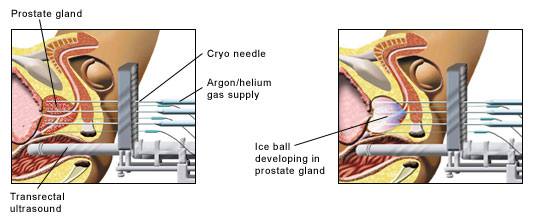
Cryosurgery is a technique designed to destroy the prostate gland in a minimally invasive way utilising cryogenic gas. It can be used for men with prostate cancer confined to the gland and also in men where the prostate cancer is locally advanced ie on the edge of the gland. In the United Kingdom it is mainly used for men who have recurrent prostate cancer following radiotherapy treatment (either external beam or brachytherapy).
Although minimally invasive it is a procedure requiring expertise in prostatic ultrasound scanning, cryo-needle placement and experience in monitoring ice ball formation.
Cryosurgery is also referred to as cryoablation or cryotherapy. It is a technique that involves using cryogenic gases circulated through tiny cryoprobes or needles within the prostate introduced through the skin. It is a minimally invasive technique. The concept of using extreme cold for prostate cancer was developed in the 1960’s when liquid Nitrogen was used to freeze the prostate in an unsophisticated manner. Its use was limited by complication rates and unsatisfactory results.
However, introduction of liquid argon and helium gas technology, linked to sophisticated prostate ultrasound scanning techniques, has allowed cryosurgery to develop in a manner that minimises complications and improves results.
The prostate tissue is frozen to -140ºc using argon gas and warmed using helium gas. Fine cryoneedles are introduced through the perineum, the area between the scrotum and anus, under ultrasound controlling using a template guide for accuracy. There are no incisions. Temperature needles are used to monitor the process particularly around the sphincter muscle below the prostate and also the wall of the rectum. A warming catheter is used throughout the procedure to protect the inner lining of the urethra and sphincter muscle area.
Cryosurgery can be used for men with prostate cancer which is localized to the gland, just on the edge of gland (locally advanced) and in cases were recurrence of prostate cancer occurs post radiotherapy (including brachytherapy).
Cryosurgery is best used in situations where the PSA is less than 15 and the Gleason grade of the pathology grade 7 or below.
Men who have severe urinary symptoms or those who have had previous prostatic surgery may not be suitable although this will be assessed at initial consultation by a questionnaire and urinary flow tests. A preliminary telescope examination under local anaesthetic and bladder pressure monitoring also under local anaesthetic may be necessary as part of the initial assessment.
Some men may have a large prostate gland which can make cryosurgery may be difficult. It is usually possible to shrink the gland using hormonal agents which are often used in prostate cancer treatment. This is discussed at the initial consultation if necessary.
Advantages
Cryosurgery is minimally invasive and can be carried out either as a day case or with an overnight stay. There is little in the way of post operative pain although bruising is quite common around the site of the cryoneedles in the perineal area.
Most men are up and about quickly following the procedure although it is advisable not to take strenuous exercise during the period whilst the catheter is in place.
There is usually no need for a transfusion as blood loss in minimal. Cryosurgery can be repeated at a later stage if necessary.
Cryosurgery can be used for men who have recurrence prostate cancer post radiotherapy (including brachytherapy). It can also be used in men who are unsuitable for major surgery or radiotherapy.
Focal cryosurgery has introduced in some centres particularly in the United States. This is where the tumour within the gland is identified and treated. This technique is still under review although early results are promising with regards lower impotence rates.
Disadvantages
The technique has a higher risk of impotence than other treatments as the nerves for erection lie just behind the gland adjacent to the rectum and are included in the freeze process. Recovery can occur however over twelve months. Patients can be instructed in the use of medications such as such as Viagra, injection therapy and vacuum erection devices if necessary.
Pre-operation
On admission the procedure is discussed both with the surgeon and with the anaesthetist. The procedure can be carried out either under a general anaesthetic or using a local anaesthetic ie spinal. Patients are usually given a simple enema to clear the lower bowel.
The procedure takes between 1 ½ and 2 hours. Intravenous antibiotics are given to guard against the risk of infection.
Cryoneedles are introduced through the perineum under ultrasound guidance and a computer technique utilising a template grid. Full temperature monitoring is carried out and the urethra is warmed to preserve the sphincter muscle.
Post operation
When the patient awakes he will have a urethral catheter draining through the penis. This allows swelling of the prostate to settle in the 14 days or so following the cryosurgery. There are dressings around the perineum to minimise bruising. The patient is returned to the ward and later instructed how to use the catheter. The patient is discharged with dressings which are changed daily following a bath. Simple pain killers may be necessary to relieve discomfort although this is usually quite minimal.
Discharge from hospital
Patients are given instructions on care of the catheter and will be discharged with antibiotics for one week and also medication known as alpha-blockers which are usually taken once a day. These aid with the removal of the catheter.
A follow up by telephone will be arranged through the surgeon and the cryosurgical nurse specialist. Usually men are reviewed at six weeks when an examination is carried out and the PSA measured.
Constipation is quite common following any surgical procedure and is usually managed by simple means such as gentle laxatives and increased fluid intake.
Bruising around the perineum area is common and managed by simple dressings and avoiding prolonged periods of standing in the two weeks following cryosurgery.
Blood in the urine is very common following catheter insertion and removal and can occur for intermittently for several weeks after cryosurgery.
Longer term problems include urinary incontinence particularly during coughing and sneezing (stress incontinence). Patients are discharged following catheter removal with simple pads to minimise discomfort and are given full instructions in pelvic floor exercises.
Impotence
This is a common problem following cryosurgical treatment and will have been discussed in detail before consideration of cryosurgery. Recovery is possible over twelve months or so. There are various ways of helping with this problem and these are usually discussed pre-operation with the surgery and cryosurgery nurse specialist.
Post cryosurgery and removal of catheter
Men can return to normal activities following catheter removal. It is advisable to continue pelvic floor exercises.
Pelvic floor (or Kegel’s) exercises
- To do these exercises effectively, you need to first relax your abdominal and buttock muscles.
- To identify and correctly contract the pelvic floor muscles, imagine that you are trying to hold back bowel movements or from passing gas.
- During this action, you should feel the opening of the rectum contract.
- Tighten the muscles for 3-5 seconds and then relax for 6-10 seconds. Repeat this sequence 20-25 times.
- Do the set of 20-25 contractions 3-4 times daily.
During the first week of the programme, perform the exercises whilst lying down, but later while sitting and standing. After the initial learning period, perform the exercises when you need them, i.e. just before sneezing, coughing or straining.
Cryosurgery is an effective treatment for men who have evidence of recurrence of prostate cancer following treatment utilising external beam irradiation or brachytherapy. Staging investigations however are essential to check that the disease remains confined to the gland. It has been reviewed and approved by the National Institute of Clinical Excellence (NICE).
Cryosurgery for localised (early) prostate cancer indicates that the results are as effective following those with radical surgery and radiotherapy. However the impotence rate is higher as the nerve areas are frozen during the procedure. NICE is at present reviewing the literature for its use in localised prostate cancer. A decision is due late 2005.
Cryosurgery is a technique requiring considerable skill in ultrasound scanning of the prostate and needle placement. In addition, as with all surgical techniques, best results are obtained by surgeons who have carried out a large number of these procedures. This should be discussed with the surgeon before making a final decision with regards treatment.






