Download the Prostate Cancer Centre's printable PDF booklets to read offline.
Prostate Cancer - General information
Prostate Cancer - Brachytherapy
Prostate Cancer - Radical Prostatectomy
Prostate Cancer - External Beam Radiotherapy
Use the Prostate Cancer Centre's treatment selector to get an idea of what treatment is right for you.
Select this link to view the treatment selector
©The Prostate Cancer Centre UK Ltd 2005. All rights reserved.

Radical Prostatectomy
Radical prostatectomy is an operation performed to remove the entire prostate and is only done for cancer which is thought not to have spread beyond the prostate (organ-confined). It should not be confused with transurethral (performed through the penis, using a telescope) prostatectomy (TURP), which removes only the inner two-thirds of the prostate and is performed for a prostate obstructing the flow of urine from the bladder. It is a major operation with an excellent safety record when done by an expert.
Radical prostatectomy was first performed over a century ago, although it has only been widely used as a treatment for localised prostate cancer worldwide for the past 20 years, and in the UK for the past 10 years. This is due to the development of PSA testing allowing cancers to be detected at an early stage, together with the fact that the operation is technically demanding and surgeons require considerable training before having the necessary skills to safely perform such surgery.
Radical prostatectomy is now the commonest major urological procedure performed in many specialist hospitals in the UK. It can be performed by any of three routes:
- Retropubic
- Perineal
- Laparoscopic (keyhole)
Retropubic
This is the commonest approach for open (i.e. non-keyhole) prostatectomy and involves an incision in the lower part of the abdomen, typically from just below the umbilicus (belly button) to just above the penis. The advantages of this route are that the lymph nodes (see page 5) can be removed if they need to be and that this is a surgical approach familiar to all urologists. The disadvantages of this approach are: the relatively awkward operative access to the prostate, which is partly hidden by the pubic bone; bleeding (which requires blood transfusion in about two-thirds of patients); and post-operative discomfort from the wound.
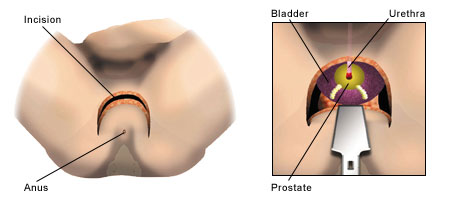
Perineal
This is less commonly performed than retropubic prostatectomy, because of the lack of familiarity of this route to most urologists. It is done through an incision between the anus and the scrotum (the perineum). Its advantages are less bleeding and better access to the prostate, which is located just beneath the perineum. Its disadvantages are the inability to remove the lymph nodes (if necessary), its lack of suitability for large prostates (because of confined space) and the greater risk of rectal problems during and after surgery.
Laparoscopic

This approach has attracted great interest since 2000, but is still performed by only a few urologists in the UK due to the small number of units able to train surgeons. Nevertheless, this procedure is becoming increasingly popular with surgeons, and requested by patients, and points the way for this type of operation in the future. This technique combines the advantages of retropubic prostatectomy with better vision for the surgeon and reduced blood loss, hospitalisation, catheterisation time and recovery. It is done through five 1cm incisions in the abdomen. The only disadvantage of this approach is that it takes longer to perform and is technically more demanding.
- The true stage (extent) and grade (aggressiveness) of the cancer can be determined.
- If the cancer is confined to the prostate, and the entire gland is removed, surgery should be curative.
- The prostate-specific antigen (PSA) blood test should fall to zero within 4 weeks of surgery and remain undetectable.
- If prostate cancer recurs, the PSA will detect this between 3-5 years before symptoms occur, and radiotherapy can be given.
- Surgery corrects any obstruction to the flow of urine from the bladder caused by enlargement of the prostate that may give rise to urinary symptoms such as a poor urinary stream and the need to get up at night to pass urine.
Wound discomfort
The wound resulting from radical prostatectomy normally heals well within 10 days and the discomfort soon fades. The wound from the retropubic approach is the most uncomfortable, followed by the perineal technique. The laparoscopic technique causes the least discomfort; hence its appeal. Nevertheless, whichever approach is used, wound problems are uncommon and any discomfort can be effectively controlled by painkillers.
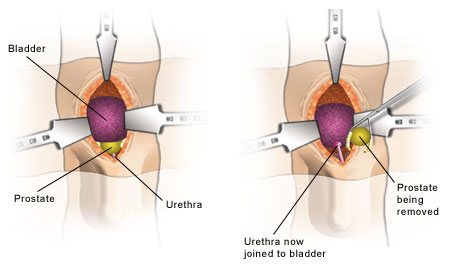
Urine incontinence
Leakage of urine on coughing, sneezing, laughing and standing up may initially occur, following removal of the catheter (a tube that drains urine from the bladder into a bag). This is known as ‘stress’ incontinence and is managed by wearing absorbent pads. It is present because the urethra (tube you urinate through) and bladder are brought together by sutures (stitches) at the end of the operation. This process causes bruising, swelling and impaired function of the sphincter (continence valve). The younger, fitter and slimmer the patient, the faster continence returns. Exercises to strengthen the pelvic floor also hasten continence. Continence rates differ amongst surgeons. Good continence rates would be 70% of patients pad-free at 3 months after surgery, 85% after 6 months and 95% after 12 months. The 5% of patients not pad-free at 12 months are offered insertion of an artificial sphincter. This involves a smaller operation, to implant it, and carries a high success rate.
Risk of impotence
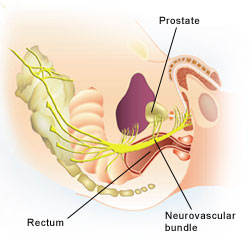
Most surgeons advise against preserving the neurovascular (nerve and blood vessel) bundles, which travel on either side of the prostate to allow spontaneous erections, in men who are already impotent, are over 70 years (because of the risk of impending impotence) or have prostate cancer at high risk of spreading outside of the gland.
This is because the first route of escape of prostate cancer out of the prostate is via the nerves, which lie in contact with the prostate and penetrate its capsule every centimetre or so. However, even if these nerves are intentionally removed, which removes spontaneous erections, it is important to remember that all men can be made potent following radical prostatectomy somehow.
All other patients are offered nerve-preserving prostatectomy. Again, the younger and fitter the patient, the faster erections return. This process may take up to 2 years in some patients. Potency (erection) rates differ amongst surgeons. Good potency rates would be 50% of patients, at 12 months after surgery.
All patients with organ-confined prostate cancer, a PSA of 15ng/ml or less and a Gleason score of 8 or less are suitable. Patients with a PSA of over 10ng/ml need a CT or MRI (body) scan, and patients with a PSA over 15ng/ml need a bone scan to confirm that the prostate cancer is organ-confined. Patients who are in poor general health, are very overweight or have existing cardiovascular or breathing problems may be better suited to other forms of treatment.
Patients who have had previous prostate surgery, such as a TURP, or who have troublesome urinary symptoms, such as a poor urine stream, are often best suited for this form of treatment for their prostate cancer, when the prostate gland causing their symptoms is removed.
Before the operation
Patients are given written instructions on pelvic floor exercises and advised to start them as long as possible before surgery. Routine pre-operative (blood, urine and ECG) tests are done either 10-14 days or the day before surgery, depending on how far you live from the hospital. You will be visited by your anaesthetist and surgeon before the operation to answer any remaining questions and obtain your written consent.
The procedure
This will take 2-3 hours to perform, depending on the degree of difficulty. During this time, the prostate and seminal vesicles are removed, the neurovascular bundles preserved and the lymph nodes removed (in low- and high-risk cases, respectively). The bladder and urethra are then sutured together over a catheter and a drain inserted.
After the operation
When you wake from the anaesthetic in the Recovery Room, you will have a catheter in the penis, a drain in your abdomen and at least one drip in your arm. You should expect some discomfort, but this can be easily controlled, using the painkilling drugs you will be offered. Patients undergoing open surgery may have a blood transfusion and/or an epidural catheter, to numb all sensation from the waist down. This is usually removed after 1-2 days.
Patients are allowed to eat and drink on the first day following surgery. They are discharged home with their catheter after 2-7 days and are re-admitted 10-21 days following surgery for catheter removal, depending on the method of surgery. An x-ray (cystogram) is requested by some surgeons prior to catheter removal. A urine sample will be taken from the catheter prior to its removal, and patients may be started on antibiotics after its removal. Patients will be allowed home once it is established that they can pass urine. Only 1% of patients have urinary retention (cannot pass urine) and need to have a catheter reinserted for another 10 days or so.
Constipation
This is common after any major operation and should not concern you. If you are particularly uncomfortable, take 2 senna tablets at night (they take 12 hours to work). Do not strain to open your bowels.
Blood in the urine
This is common both before, and for 3 weeks after, your catheter has been removed.
Continence
You will probably not be continent immediately. Caffeine-containing drinks (tea, coffee and cola) and alcohol make this worse, temporarily. The number of pads you need to use will reduce with time.
Erections
Do not be afraid to experiment with erections and sex at any time after the operation, but remember that it can take up to 2 years for erections to return and that intercourse is much easier with lubrication jelly, which can be bought without a prescription from any pharmacy.
You should also be aware that you do not need an erection to orgasm. The orgasmic sensation will still be enjoyable and fulfilling, but no fluid will come out. You will be sterile, so contraception is unnecessary.
Remember also that if erections do not return naturally, all men can be made potent somehow.
You should expect to return to most activities 4 weeks after laparoscopic and 12 weeks after open surgery. You are safe to drive as soon as you can brake hard enough to perform an emergency stop.
Your first outpatient appointment will be approximately 4 weeks after surgery, when the results of the laboratory analysis (histology) of your prostate should be available. Your first PSA test will usually be done 2 weeks before your next outpatient appointment (3 months following surgery). You will typically be seen with an up-to-date PSA test every 3 months for a year and then every 6 months for 4 years. Your GP might be asked to check your PSA annually for another 10 years, depending on surgeon preference.
Pelvic floor (or Kegel’s) exercises
- To do these exercises effectively, you need to first relax your abdominal and buttock muscles.
- To identify and correctly contract the pelvic floor muscles, imagine that you are trying to hold back bowel movements or from passing gas.
- During this action, you should feel the opening of the rectum contract.
- Tighten the muscles for 3-5 seconds and then relax for 6-10 seconds. Repeat this sequence 20-25 times.
- Do the set of 20-25 contractions 3-4 times daily.
During the first week of the programme, perform the exercises whilst lying down, but later while sitting and standing. After the initial learning period, perform the exercises when you need them, i.e. just before sneezing, coughing or straining.
Commonly asked questions (taken from The Prostate Cancer Charity Toolkit)
- Will I be given hormone treatment prior to surgery? If yes, why? If not, why not?
- How long does the operation take?
- Will I have a blood transfusion?
- How many of these operations do you do a year?
- Will you be removing anything other than my prostate?
- Will you attempt to do nerve-sparing surgery if possible? In your experience, how successful is this procedure?
- What are your results in respect of impotence and incontinence?
- How long will I be in hospital?
- Will I have much pain after surgery and how will it be controlled?
- If I go home with a catheter, when will it be removed and by whom?
- How soon is my follow-up appointment after discharge?
- If I have continence problems after the surgery, how would these be managed and by whom?
- How often will my PSA be checked?
- What should the PSA be after surgery? What would it mean if it doesn't reach that level? What would you do then?
Radical prostatectomy is a very effective treatment for early prostate cancer. Following it, PSA values should be zero, as the prostate has been removed. An unrecordable PSA value 5 years following surgery indicates cure. Persisting side-effects of radical prostatectomy can be effectively treated or eliminated. Laparoscopic radical prostatectomy is a technically elegant way for the prostate to be removed, but requires extensive specialist training before it can be safely performed.
The only important factor influencing the result of your radical prostatectomy which you can change is your surgeon. Choose him or her with care.
We have collected stories from our patients who have undergonesome of the treatments offered at the Prostate Cancer Centre.






